Functional Endoscopic Sinus Surgery (FESS)
What are the Paranasal Sinuses?
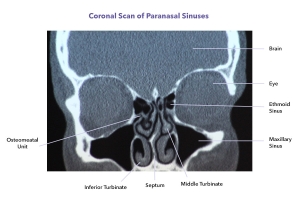
The paranasal sinuses are air cavities within the bones of the face and skull that connect to and ventilate via the nasal cavity. Their function is not really known, they may exist to make the head lighter or to protect the brain from frontal impact much like the crumple zone in a car. Regardless they not infrequently cause problems.
What is required for healthy paranasal sinuses?
The sinuses are air spaces but are lined with a layer of tissue that produces a thin mucus blanket that coats the walls of the sinuses. This lining tissue has microscopic hairs called cilia that sweep the mucus out along designated pathways through the natural drainage holes (ostia) into the nasal cavity and then into the throat where they are swallowed.
If this mucus blanket fails or the Ostia is/are obstructed sinus disease can result.
What is FESS?
Functional endoscopic sinus surgery is the modern approach to surgery on the sinuses. In the past operations were designed to maximise drainage by gravity. As such large holes were fashioned into the sinuses and most of the lining tissue was removed. It is now known that this lining tissue plays a critical role in keeping sinuses healthy. As such the old-style surgery not infrequently worsened the problem.
Functional endoscopic sinus surgery places an emphasis on function. Given that we now know how important the normal anatomy and lining of the sinuses are to sinus health, the surgery is all about establishing ventilation and drainage along the normal pathways with maximum preservation of normal structures and in particular the sinus linings. The surgery is now a minimal rather than an extensive destructive procedure.
The availability of high definition cameras and very fine endoscopes allows for much greater control during the surgery and hence significantly better results.
Indications for FESS
Functional endoscopic sinus surgery may be indicated in the following common conditions;
The operation
Functional endoscopic sinus surgery is performed in hospital, usually under a general anaesthetic but can be performed with local anaesthesia and intravenous sedation.
Using fine endoscopes and high-definition cameras it is possible to obtain an excellent view. The area that most frequently needs to be dealt with is called the ostiomeatal unit. It is an area on the sidewall of the nose where many of the sinuses drain. By removing a small amount of bone in this area improved ventilation and drainage can usually be achieved. Not infrequently there are anatomical variations in this area that make people prone to sinus disease. These can be readily corrected at surgery. In more extensive sinus disease there may be a need to operate on other sinuses such as the sphenoid and frontal sinuses.
Not infrequently this surgery will be performed in conjunction with Septoplasty or Turbinate Surgery.
A light pack may be placed in the nose at the end of surgery to help with bleeding.
After surgery
The first night
An overnight stay in hospital is normal after the surgery. It is not uncommon have a small amount of bleeding on the first night. Pain is not normally a major feature.
Discharge from hospital
Around 7 AM the following morning the nursing staff will remove any packs. It is not uncommon to have a slight bleed at this point. I will usually be in around 730 AM to make sure all is well. Providing there are no concerns with bleeding or nausea discharge would normally occur mid-morning.
Diet
Following nasal surgery it is best to avoid food and drinks are too hot as they may increase bleeding. A cool to warm normal diet is satisfactory.
Activity
Because the nose is such a vascular structure excessive physical activity may provoke bleeding. I therefore suggest that strenuous physical activity is avoided for two weeks.
Pain relief
Pain is not normally excessive following FESS however nasal congestion and mild to moderate headaches are not uncommon. Surgery on the nose results in the release of natural compounds called inflammatory mediators. These are the same compounds that are released in viral infections and it is not at all unusual to have symptoms similar to a virus.
Paracetamol is normally sufficient however Palexia is also prescribed in case it is required. Nurofen should not be used.
Other medications
I normally also prescribe antibiotics to be used for one week.
Salt-water nasal sprays or douches are also provided and help clear some of the mucus and congealed blood.
Nose blowing
It is best to avoid nose blowing from the first few days as excessive or vigorous nose blowing may precipitate bleeding. Thereafter the noise may be blowing gently, both nostrils at the same time.
Nasal obstruction
It is normal to have some nasal obstruction for several days to a week following Nasal Surgery. This is due to swelling and congestion in a confined space. Sleeping with the head elevated may help to some degree.
Bleeding
It is normal to have bloody mucous discharge from the nose or an occasional small fresh bleed for a few days after the operation. If bleeding is heavy or prolonged you should contact me.
Postoperative instructions
You will be given instructions for care upon discharge. These are also available to download here. At discharge you will also be given a post-operative appointment and my mobile phone number.